Another common scenario is when a worried mum calls asking that a doctor listens to her child’s chest and the child has a rattly cough. The parent hears the rattling or sometimes feels it as holding the child back and she starts to worry that it might be a sign of chest infection.
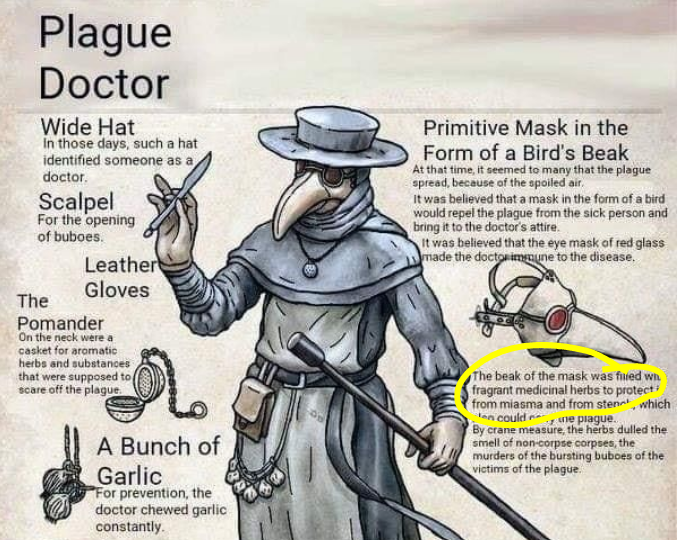
Again, I think there is an overestimation of how much a doctor can do with a stethoscope. I know that the stethoscope is the symbol of medicine as the wide hat was in the Middle Ages and doctors don’t rush to disperse the myths around it, however it is particularly useless when assessing for children’s pneumonia. Other factors together, like high temperature longer than 5 days, not feeding, not drinking, signs of breathing difficulty, ribs or tummy sucking in, high breathing rate per minute and how the child looks and behaves in general give you a much better chance to diagnose pneumonia in children than the stethoscope.
Even worse when the parent expects the doctor to be able to tell how the child will be in 3 days time when the family is leaving for a holiday. I am really sorry, I am just a doctor and can only tell whether the child needs medical intervention right now, and I only have a stethoscope not a crystal ball to see what will happen in the future. We need to take it day by day and if the child develops any of the above worry signs they need to be reassessed.
All this information about chest infection and what a doctor can and cannot do might come to you as a massive shock, but yes, medicine has its limitations and the stethoscope is not a magic wand even if we doctors tend to use it like that…
It is time to demystify medicine and use it wisely.
I hope you will get better soon!